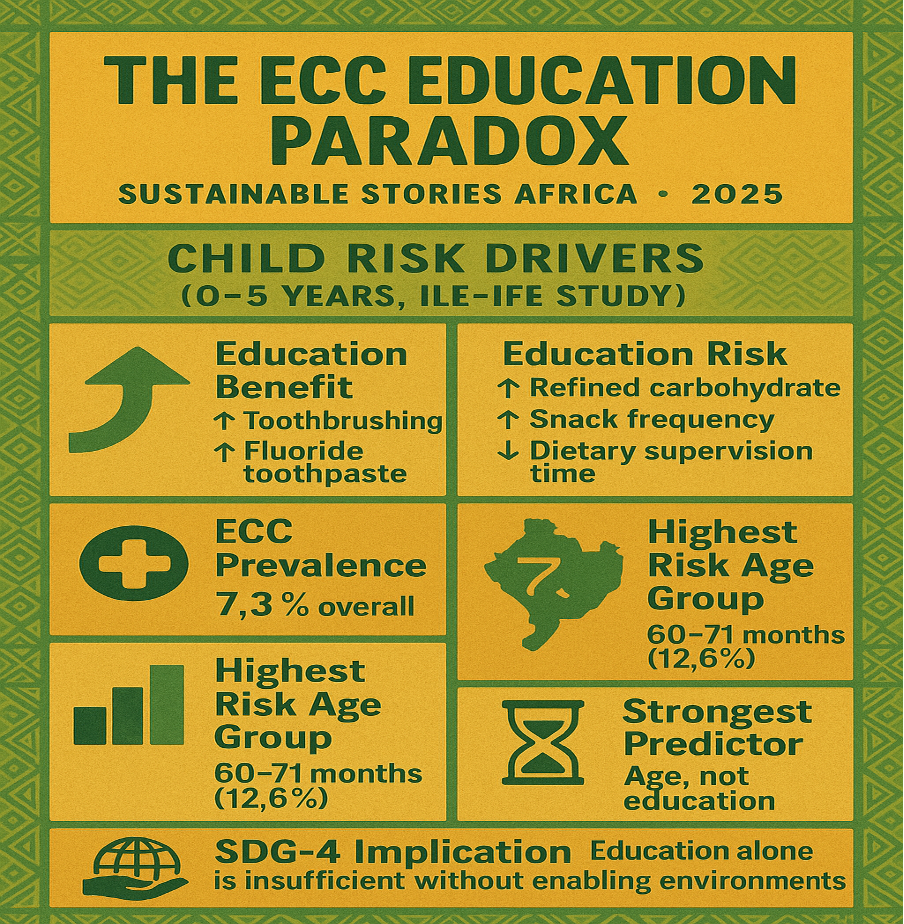
Early childhood caries (ECC) remains one of Nigeria's silent child-health crises, and new evidence from Ile-Ife reveals a troubling paradox: higher parental education improves brushing and toothpaste choices but also increases children's refined carbohydrate consumption.
Education Raises Hope, Risk Remains Unmoved
Nigeria's childhood-health landscape is evolving quickly, yet one statistic from Ile-Ife stands out with unusual clarity: 7.3% of children aged 0–5 years now live with early childhood caries (ECC), a 55% increase over five years. Behind this number lies a deeper social tension: Does education actually protect children from preventable oral disease?
A study, grounded in the SDG-4 framework, followed 1,339 mother–child pairs and mapped how parental education shapes brushing habits, sugar exposure, and dietary risks.
The findings reveal a counterintuitive picture: educated mothers and fathers adopt more protective practices, such as regular brushing and fluoridated toothpaste use, but at the same time, their children consume more refined carbohydrates between meals, a major ECC driver.
The result is a complex behavioural landscape where education does not directly lower ECC prevalence. Instead, environmental pressures, cultural norms, and Nigeria's increasingly "snack-saturated" food ecosystem blunt the potential benefits of schooling.
This article interprets these findings through Sustainable Stories Africa's lens – placing children's lived realities, parental choices, and structural gaps at the centre of a national conversation about oral health equity.
When Learning Fails to Shield Smiles
Nigeria's path toward SDG-4 paints education as a powerful equaliser, yet the latest oral-health evidence from Ile-Ife presents a compelling contradiction: education improves parental knowledge but does not reduce ECC prevalence.
The expectation that tertiary schooling should dramatically reduce early childhood caries is not supported by the data. In reality, children of secondary-educated fathers had the highest ECC prevalence (9.0%), while tertiary-educated fathers recorded the lowest (4.2%), a statistically significant divide.
Meanwhile, mothers with tertiary education demonstrated lower caries prevalence in their children (4.8%), but the association was not statistically significant. The result challenges long-held assumptions about parental education as a predictable protective factor.
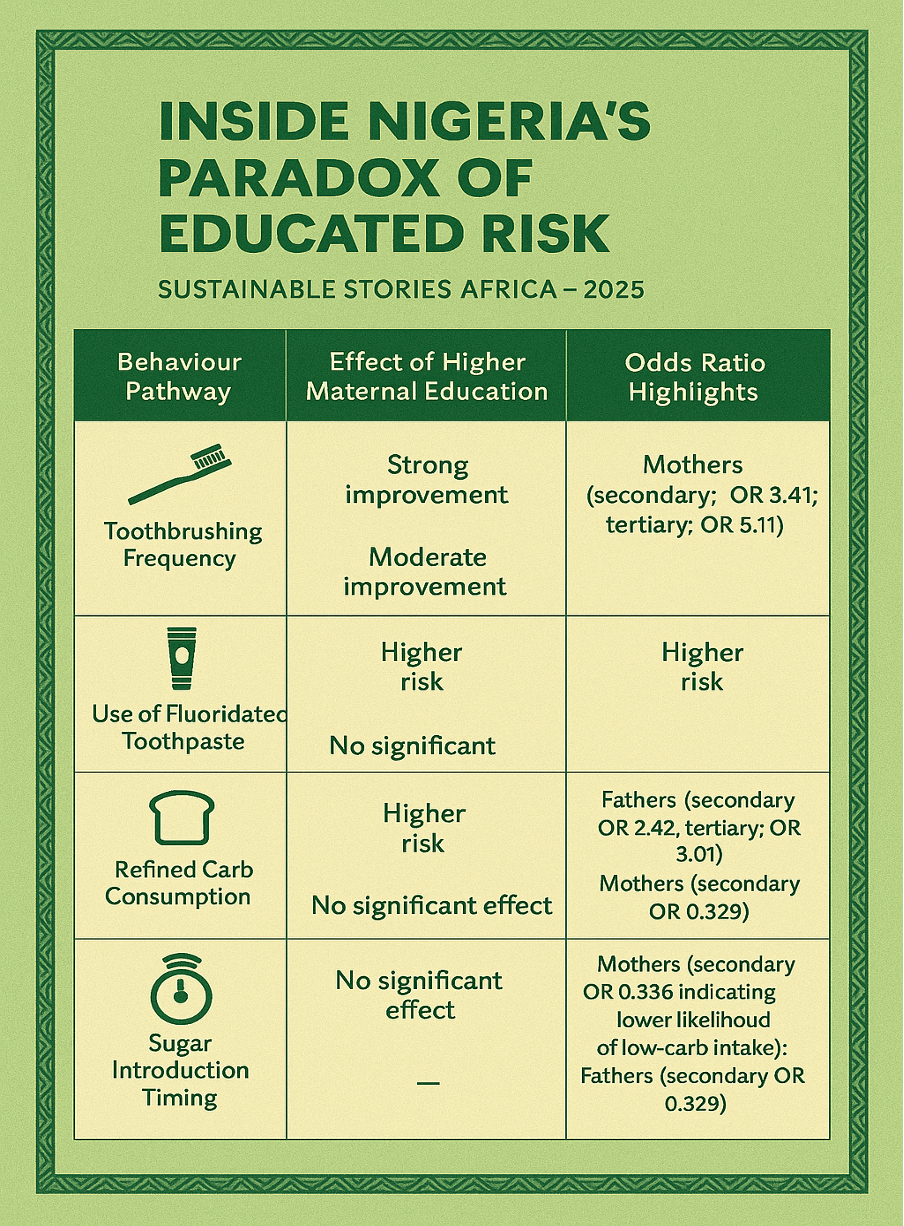
Inside Nigeria's Paradox of Educated Risk
- Behavioural Pathways Tell a Different Story – The behavioural paradox emerges clearly: parents with more education practice better hygiene but feed children more refined carbohydrates, likely due to lifestyle factors, such as work schedules, affordability of convenience snacks, increased disposable income, and modern food environments that reward speed over nutrition.
The study highlights that education improves some behaviours but worsens others:
| Behaviour Pathway | Effect of Higher Maternal Education | Effect of Higher Paternal Education | Odds Ratio Highlights |
|---|---|---|---|
| Toothbrushing Frequency | Strong improvement | No significant effect | Mothers (secondary: OR 3.41; tertiary: OR 5.11) |
| Use of Fluoridated Toothpaste | Moderate improvement | Strong improvement | Fathers (secondary: OR 2.42; tertiary: OR 3.01) |
| Refined Carb Consumption | Higher risk | Higher risk | Mothers (secondary OR 0.336 indicating lower likelihood of low-carb intake); Fathers (secondary OR 0.329) |
| Sugar Introduction Timing | No significant effect | No significant effect | — |
- Age and Environmental Influence Matter More Than Education – ECC prevalence climbs sharply with age:
- 1.6% among infants 0–11 months
- 12.6% among children 60–71 months
Age, not parental education, remains the dominant predictor.
The study thus reinforces oral health as a product not only of what parents know, but what the environment allows them to practice.
The ECC Education Paradox
Reimagining Education as Everyday Protection
The findings call for a shift in how Nigeria interprets the power of education in health outcomes. If education alone does not shield children from caries, then public health interventions must respond in layered, locally grounded ways.
The article's evidence suggests several positive directions:
- Holistic SDG-4 Alignment – Education must include oral-health literacy integrated in early childhood centres and primary schools.
- Parental Empowerment Beyond Knowledge – Both fathers and mothers require actionable tools—not just awareness. Examples include:
- Subsidised fluoride toothpaste
- Community snack-choice guides
- Local workshops on balanced feeding practices
- Environmental Transformation – Nigeria's obesogenic environment—dominated by cheap refined snacks—overpowers parental intentions. Policies such as:
- Sugar-sweetened beverage taxes
- Regulated snack advertising to children
- Incentives for healthier school snacks can help match education with accessible, healthier options.
Protecting the Most Vulnerable – Children of less-educated parents face the greatest structural barriers, requiring:
- Mobile oral-health clinics
- Expanded community-health worker programmes
- Early caries detection campaigns at immunisation centres
With ECC rising by 55% in the community within five years, inaction carries high costs, developmental, nutritional, and economic.
From Research to Reality: The Parenting Shift Nigeria Needs
The study provides evidence for a multi-stakeholder framework:
- Government
- Implement Nigeria's National Oral Health Policy (2024–2029) with urgency.
- Legislate sugar taxes to fund preventive care.
- Education Sector
- Deploy oral-health modules through teacher-training colleges.
- Integrate brushing routines in early-years curricula—mirroring global best practice.
- Communities
- Local councils can train community health workers to deliver oral-health counselling.
- Faith and market groups can host nutrition dialogues, especially for working mothers.
- Private Sector
- Toothpaste manufacturers can partner with schools for subsidised fluoride access.
- Nigerian snack-producing companies must be pushed toward reformulation and responsible marketing.
- Parents
- Fathers should take more active roles in food purchasing and daily supervision.
- Mothers should reinforce delayed sugar introduction and resist high-frequency snack habits.
PATH FORWARD – Smarter Education, Stronger Habits, Healthier Smiles
Nigeria stands at a turning point where education must translate into healthier daily behaviours for children. The evidence is clear: parental schooling improves hygiene, but environmental and cultural pressures undermine dietary discipline.
The next phase requires integrated interventions, such as school-based oral-health curricula, sugar-control policies, and targeted parent empowerment, to close the knowledge–behaviour gap.
By aligning SDG-4 education goals with real community needs, Nigeria can transform rising ECC trends into a sustainable pathway for child-health equity.