Zimbabwe's healthcare crisis is often framed as a funding or staffing challenge. However, a quieter constraint, unreliable electricity, is undermining care delivery across clinics, rural hospitals and maternity wards nationwide.
When Electricity Becomes Clinical Infrastructure
Electricity has become as essential to healthcare as medicines and trained staff. In Zimbabwe, frequent power cuts are forcing clinics to close before sunset, disrupting emergency care, compromising vaccine storage and limiting diagnostic services—particularly in rural and peri-urban areas.
According to the International Renewable Energy Agency (IRENA), nearly one-third of Zimbabwe's 1,848 health facilities lack reliable electricity, while 42% of grid-connected facilities experience outages exceeding 12 hours daily.
The result is a health system operating below capacity, despite rising demand and expanding service mandates.
A new pathway is emerging. Decentralised renewable energy (DRE), anchored by solar photovoltaic systems, offers Zimbabwe a practical, cost-effective solution, one that aligns public health goals with energy security and climate resilience.
Why Energy Is Healthcare's Hidden Bottleneck
Zimbabwe's healthcare delivery model is built around primary facilities: clinics, rural hospitals and district hospitals that serve as the first and often only point of care for millions. However, energy instability is quietly eroding their effectiveness.
IRENA's survey of 50 public healthcare facilities found that unreliable electricity most severely affected:
- Outpatient and emergency services (54%)
- Delivery services (50%)
- Laboratory diagnostics (34%)
Beyond clinical disruption, 52% of facilities reported degraded staff working conditions, while 28% said expectant mothers avoided post-delivery stays due to power outages, raising risks for maternal and neonatal outcomes.
In a system striving for Universal Health Coverage by 2030, power reliability has become a frontline health issue, not a background infrastructure concern.
What the Data Shows About Zimbabwe's Energy
Health Gap
Zimbabwe's healthcare infrastructure spans five tiers, yet energy reliability declines sharply outside urban centres.
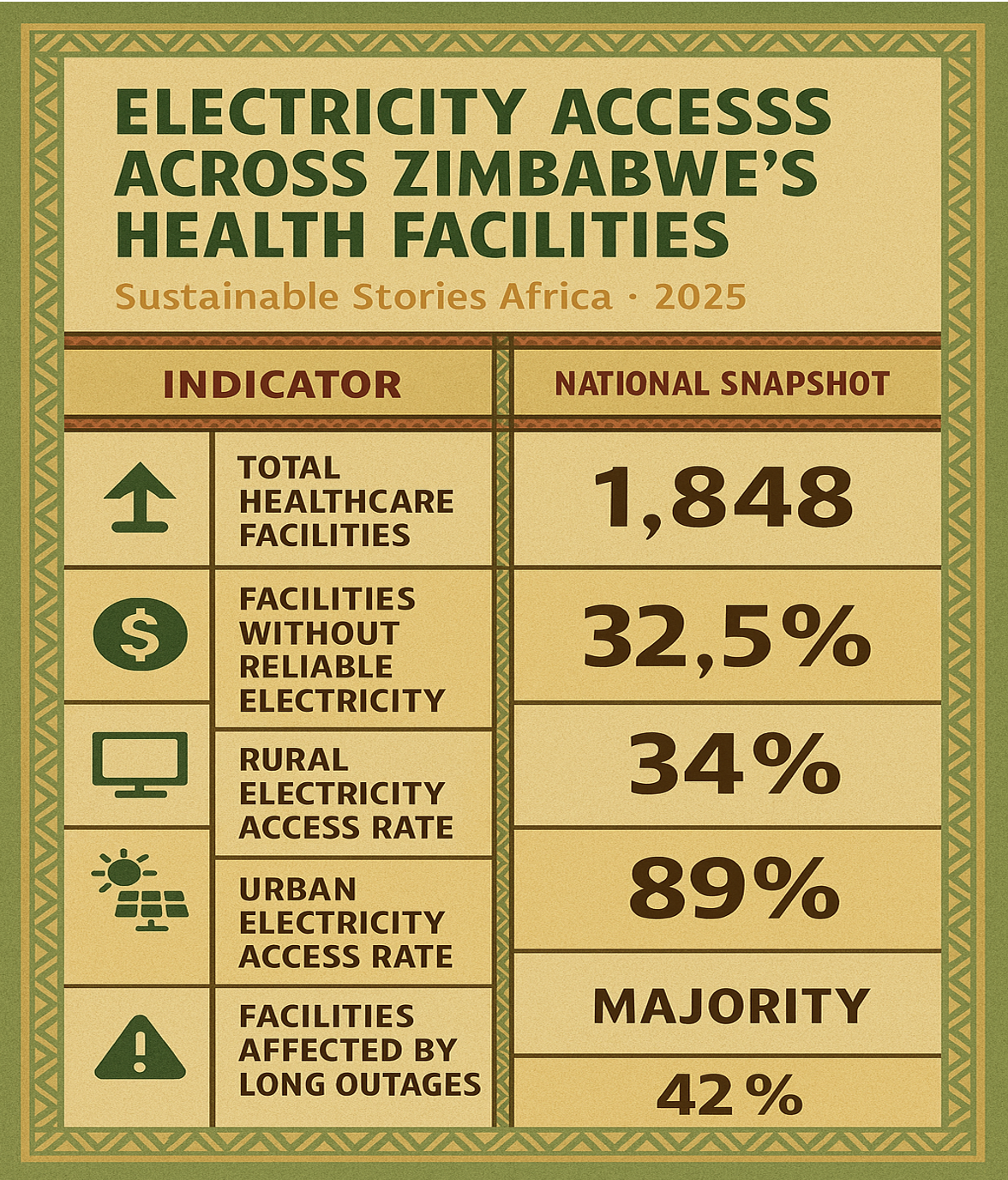
Electricity Access Across Zimbabwe's Health Facilities
| Indicator | National Snapshot |
|---|---|
| Total healthcare facilities | 1,848 |
| Facilities without reliable electricity | 32.5% |
| Rural electricity access rate | 34% |
| Urban electricity access rate | 89% |
| Facilities relying on grid + solar mix | Majority |
| Facilities affected by long outages | 42% |
Diesel generators remain common but costly and unreliable. Rising electricity tariffs, now averaging $0.1328/kWh, further strain health budgets, diverting resources from medicines, staff and facility upgrades.
Solar systems already exist in many facilities, yet poor design, limited battery capacity and weak maintenance regimes reduce their effectiveness. The challenge, IRENA argues, is not technology availability, but system design, governance and sustainability.
Why Decentralised Solar Is the Most Viable Option
IRENA's analysis identifies decentralised solar PV, paired with battery storage, as the most scalable and resilient solution for Zimbabwe's healthcare sector.
Zimbabwe's solar irradiation averages 5.7 - 6.5 kWh/m²/day, placing it among Africa's strongest solar markets. Harnessing even a fraction of this potential could stabilise power for clinics nationwide.
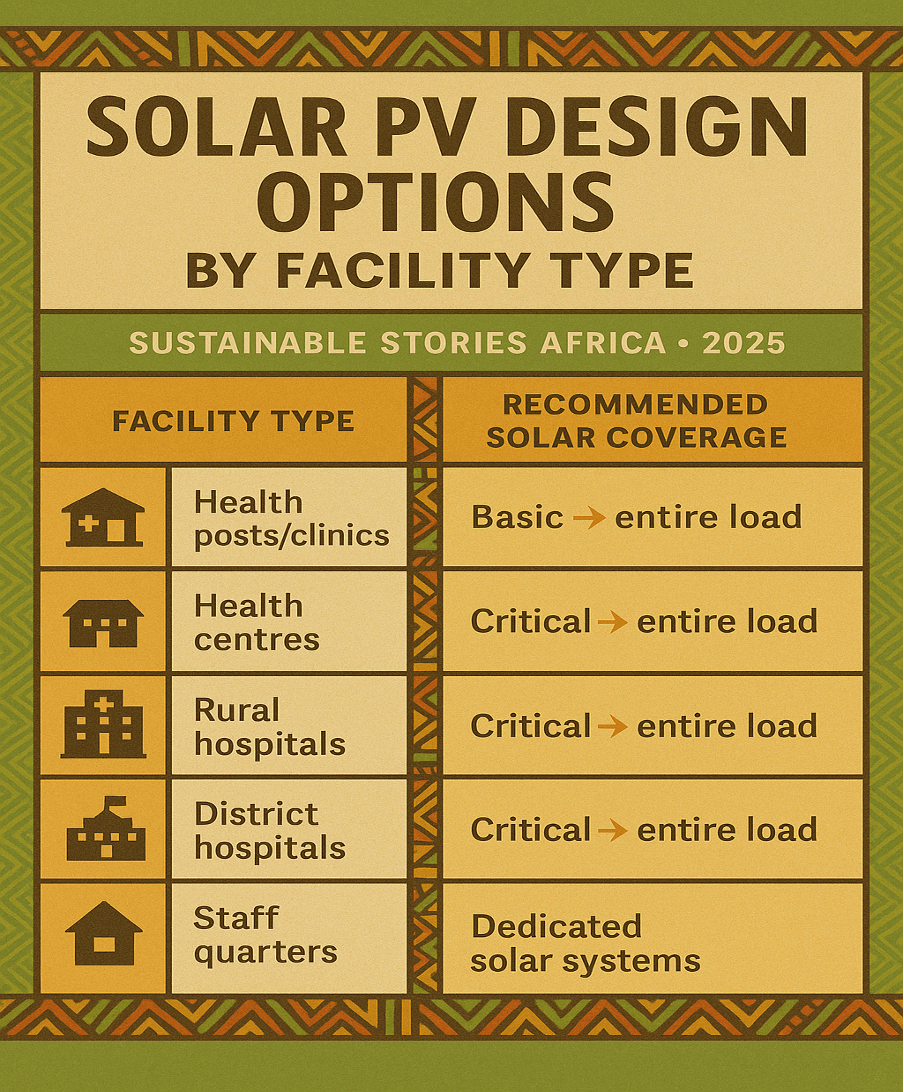
Solar PV Design Options by Facility Type
| Facility Type | Recommended Solar Coverage |
|---|---|
| Health posts/clinics | Basic → entire load |
| Health centres | Critical → entire load |
| Rural hospitals | Critical → entire load |
| District hospitals | Critical → entire load |
| Staff quarters | Dedicated solar systems |
Investment Reality Check
- $15.4 million: Powering all primary healthcare facilities and staff quarters
- $3.75 million: Powering critical loads only (1,000 facilities)
- $8.4 million additional: Upgrading lower-level facilities with maternity, labs and inpatient services
Compared with recurrent diesel costs and service disruptions, the economic case is compelling.
From Solar Installations to System Reform
IRENA's recommendations extend beyond hardware. The report calls for a health-energy ecosystem approach, anchored by:
- An interministerial committee (Health, Energy, Finance, Local Government)
- A dedicated technical programme unit overseeing quality, monitoring and O&M
- Ring-fenced funding for operations and maintenance, including out-of-warranty components
- Independent audits of existing solar assets and facility readiness
- Procurement standards aligned with WHO and international benchmarks
This model reframes energy as a long-term public health investment, not a donor-driven pilot.
What Unreliable Power Disrupts Most
- Emergency & OPD services → Delayed care, higher mortality risk
- Deliveries & maternity → Unsafe night-time procedures
- Vaccine cold chains → Reduced immunisation effectiveness
- Staff housing → Lower retention, burnout
PATH FORWARD – Powering Clinics, Strengthening Care
Zimbabwe's healthcare ambitions cannot be met without reliable electricity. Decentralised solar power offers a clear, affordable pathway to stabilise services, protect health workers and improve patient outcomes, especially in rural communities.
By embedding renewable energy into health planning, Zimbabwe can align Universal Health Coverage, climate resilience and fiscal efficiency, turning clean power into a permanent pillar of healthcare delivery.













