Mali's healthcare system is being quietly undermined by an invisible constraint: unreliable electricity. From vaccine cold chains to emergency obstetric care, power shortages are limiting what doctors and nurses can deliver—especially in rural communities where the need is greatest.
A new IRENA–SELCO Foundation assessment shows decentralised renewable energy, particularly solar PV, could decisively close this gap, improving health outcomes, reducing costs and strengthening resilience across Mali's most vulnerable regions.
When Power Determines Patient Survival
Electricity is not a luxury in healthcare; it is infrastructure. In Mali, where clinics often serve as the sole lifeline for millions, unreliable power supplies have quietly become a defining factor in whether patients receive timely, effective care. Lighting failures interrupt night-time deliveries, vaccine refrigerators shut down during outages, and diagnostic equipment sits idle.
According to the International Renewable Energy Agency (IRENA), only 75% of Mali's health facilities have reliable electricity, with stark regional inequalities masking the national average.
In northern regions such as Taoudénit and Ménaka, up to 70% of facilities lack power entirely, forcing healthcare workers to improvise under dangerous conditions.
A new evidence-based pathway is emerging. Decentralised renewable energy, particularly solar photovoltaic systems, offers Mali a practical, scalable way to stabilise healthcare delivery while advancing climate and development goals simultaneously.
Why Energy Is Healthcare's Missing Link
Power disruptions in Mali are not marginal inconveniences; they are systemic failures with direct clinical consequences. IRENA's field survey of 60 health facilities found that 93% experienced compromised services, 97% reported staff discomfort, and 81% struggled with vaccine cold-chain reliability due to electricity outages.
Maternal and neonatal care are particularly exposed. Emergency obstetric services require uninterrupted lighting, sterilisation, and refrigeration. However, many rural community health centres (CSCOMs) rely on undersized solar systems or costly diesel generators that fail during fuel shortages or mechanical breakdowns.
In a country where maternal mortality stands at 367 deaths per 100,000 live births, energy access is no longer a peripheral infrastructure issue; it is a determinant of survival.
What the Data Reveals About Mali's Health-Energy Gap
IRENA's assessment paints a detailed picture of how energy deficits intersect with healthcare delivery:
Electricity Access in Mali's Health Facilities
| Indicator | National Average |
|---|---|
| Facilities with reliable electricity | 75% |
| Facilities with unreliable supply | 20% |
| Facilities without electricity | 4% |
| Facilities primarily using solar power | 59% |
| Facilities relying on diesel generators | 10% |

While Bamako enjoys near-universal electrification, northern and remote regions face chronic shortages. Even where electricity exists, outages are frequent. Diesel generators are still widely used, raising operating costs and diverting scarce funds away from medicines, staff training, and equipment maintenance.
IRENA estimates that just 2% of Mali's solar potential could meet national electricity demand, underscoring how misaligned infrastructure, not resource scarcity, drives the crisis.
Why Solar PV Is the Most Viable Solution
The report identifies decentralised renewable energy (DRE) systems as the most cost-effective and resilient solution for Mali's healthcare sector.
Solar PV systems, paired with battery storage, can provide stable power for critical loads, lighting, refrigeration, and diagnostics without reliance on fragile grid connections.
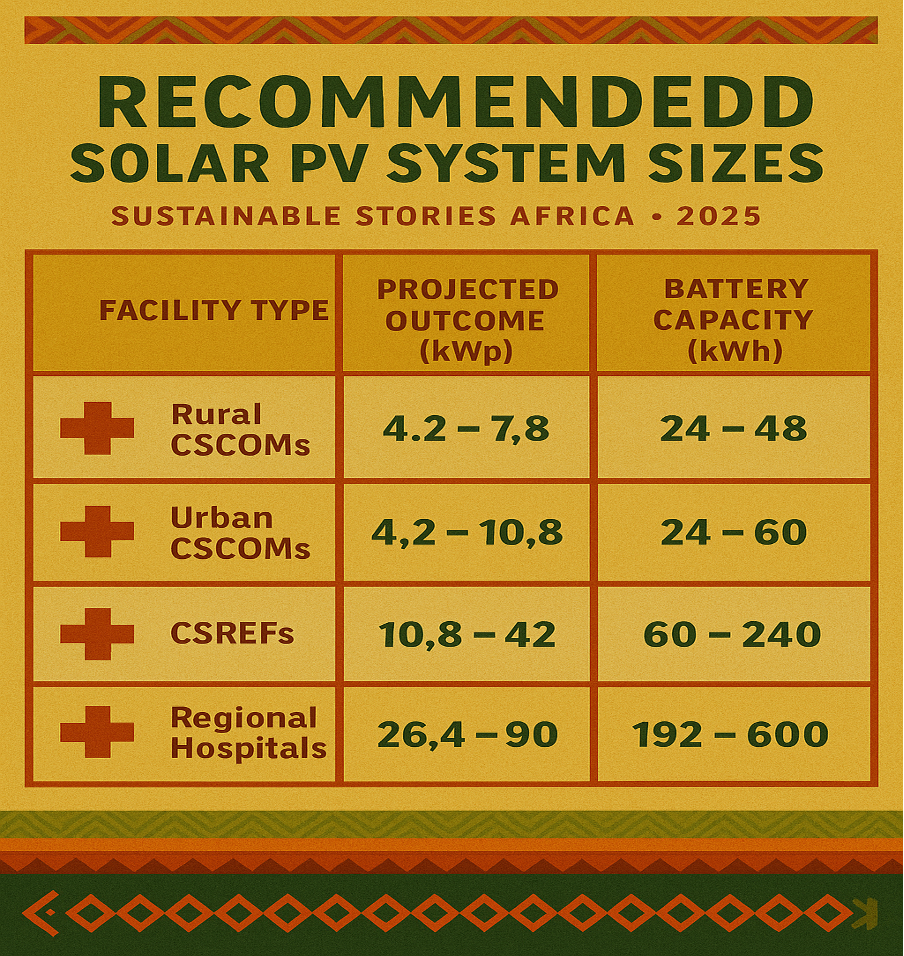
Recommended Solar PV System Sizes
| Facility Type | Solar PV Range (kWp) | Battery Capacity (kWh) |
|---|---|---|
| Rural CSCOMs | 4.2 – 7.8 | 24 – 48 |
| Urban CSCOMs | 4.2 – 10.8 | 24 – 60 |
| CSREFs | 10.8 – 42 | 60 – 240 |
| Regional Hospitals | 26.4 – 90 | 192 – 600 |
Beyond reliability, the economics are compelling. Powering all healthcare facilities and staff quarters via solar PV would cost approximately $42.1 million, while supplying critical loads alone would require $18.4 million, a fraction of long-term diesel expenditure.
Turning Energy Policy into Health Outcomes
IRENA's recommendations move beyond technology to governance and delivery:
- Establish a Solar Programme Unit within the Ministry of Health for oversight and quality control.
- Integrate long-term operations and maintenance into public health budgets.
- Prioritise local suppliers and technicians, strengthening domestic energy ecosystems.
- Phase implementation to build institutional ownership and operational resilience.
These steps position renewable electrification not as a donor-driven pilot, but as a nationally anchored health-system reform.
PATH FORWARD – Powering Clinics, Protecting Lives
Mali's healthcare crisis cannot be solved without solving its energy deficit. Decentralised solar power offers a clear, affordable pathway to stabilise services, protect health workers and save lives, especially in underserved rural regions.
By aligning energy planning with health priorities, Mali can simultaneously advance universal health coverage, climate resilience and economic efficiency, turning clean power into a cornerstone of healthcare delivery rather than an afterthought.













