Mozambique, unreliable electricity is not a technical inconvenience; it is a public-health risk. Clinics deliver babies by torchlight, vaccines spoil, and storms routinely shut down care.
A new IRENA assessment shows decentralised renewable energy can change this reality. Solar-powered healthcare is emerging as one of Mozambique's most cost-effective tools for saving lives, strengthening resilience, and protecting frontline health systems against climate shocks.
When Power Determines Patient Survival
Mozambique's healthcare system operates under intense pressure. High maternal and neonatal mortality, recurring disease outbreaks, staff shortages, and climate-driven disasters strain facilities already short of equipment and personnel. However, one constraint cuts across every challenge: unreliable electricity.
According to IRENA's 2025 assessment, only about half of healthcare facilities meet basic lighting needs, while power outages lasting up to 18 hours are common in primary health centres.
In rural clinics, diesel generators and failing solar systems often determine whether vaccines remain viable, surgeries proceed, or mothers give birth safely at night.
This SSA feature article examines how decentralised renewable energy (DRE), especially solar photovoltaic systems, can transform healthcare delivery in Mozambique.
It explores why energy access has become inseparable from health outcomes, what the data reveals about system failures, and how renewables can move healthcare from crisis management to climate-resilient service delivery.
Healthcare Without Reliable Power
Mozambique has 1,769 healthcare facilities, nearly 90% provide primary care and serve a population of about 34 million people. However, energy insecurity remains widespread.
IRENA's facility-level assessments show:
- 40% of facilities are not grid-connected
- 25% rely heavily on diesel generators
- Voltage fluctuations regularly damage equipment
- Clinics deliver babies using torchlights during outages
Climate shocks amplify these weaknesses. Cyclones Idai, Kenneth and Freddy alone destroyed or damaged over 120 health facilities, cutting off essential services when they were needed most.
In this context, electrification is no longer a background infrastructure issue. It is central to survival.
What the Data Shows About Energy and Health
IRENA's assessment of 40 representative primary healthcare facilities across six provinces reveals how deeply energy gaps undermine care delivery.
Energy Challenges in Mozambique's Primary Healthcare
| Issue | Evidence from Facilities |
|---|---|
| Power outages | Average 4 hours; up to 18 hours |
| Off-grid reliance | 86% of off-grid facilities are rural |
| Equipment damage | Voltage fluctuations damage pumps, computers |
| Vaccine risk | Refrigeration frequently compromised |
| Maintenance gaps | Lack of funds and skilled technicians |
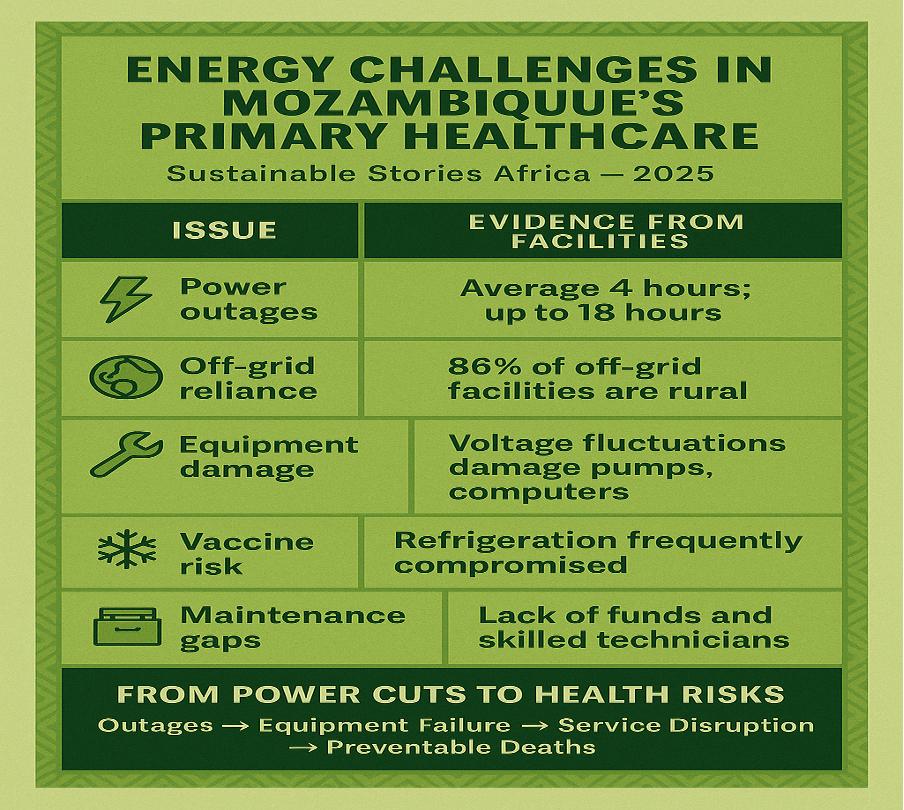
These failures translate directly into outcomes: lower immunisation rates, delayed diagnostics, unsafe deliveries, and demoralised staff, especially in remote areas where 62% of the population must travel over 12 km to reach care.
Why Renewables Are the Logical Health Solution
IRENA's conclusion is unambiguous: decentralised solar energy is the fastest, most resilient solution for Mozambique's healthcare system.
Unlike grid expansion, solar PV systems can be:
- Deployed modularly
- Tailored to facility load profiles
- Resilient to grid failure and fuel shortages
- Scaled over time
IRENA estimates that $16.5 million could power all primary healthcare facilities nationwide with reliable solar systems, while $7.7 million could cover all critical loads as backup power.
Cost of Powering Primary Healthcare with Solar
| Scenario | Estimated Cost (USD) |
|---|---|
| All loads, all facilities | $16.5 million |
| Critical loads only | $7.7 million |
| Staff quarters (additional) | $6.6 – $17.4 million |
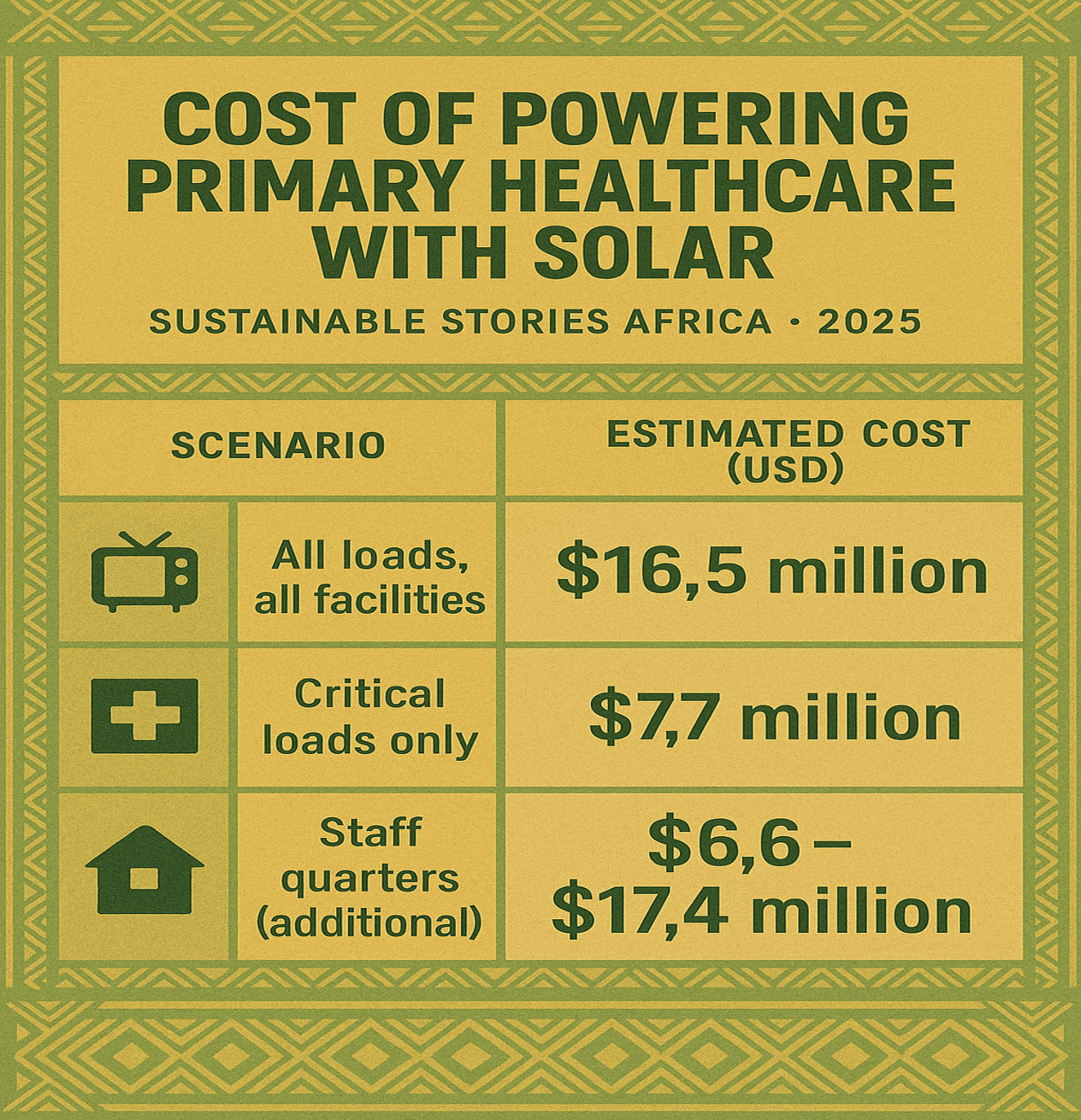
In public-health terms, this is one of the highest return-on-investment interventions available.
From Pilot Projects to System Reform
IRENA stresses that technology alone is insufficient. Past solar installations failed where maintenance, financing, and governance were ignored.
Key system reforms include:
- Inter-ministerial coordination between health, energy, and finance
- Dedicated funding for operations and maintenance
- Standardised system designs and procurement
- Training healthcare staff and local technicians
- Energy-as-a-service and PPP models
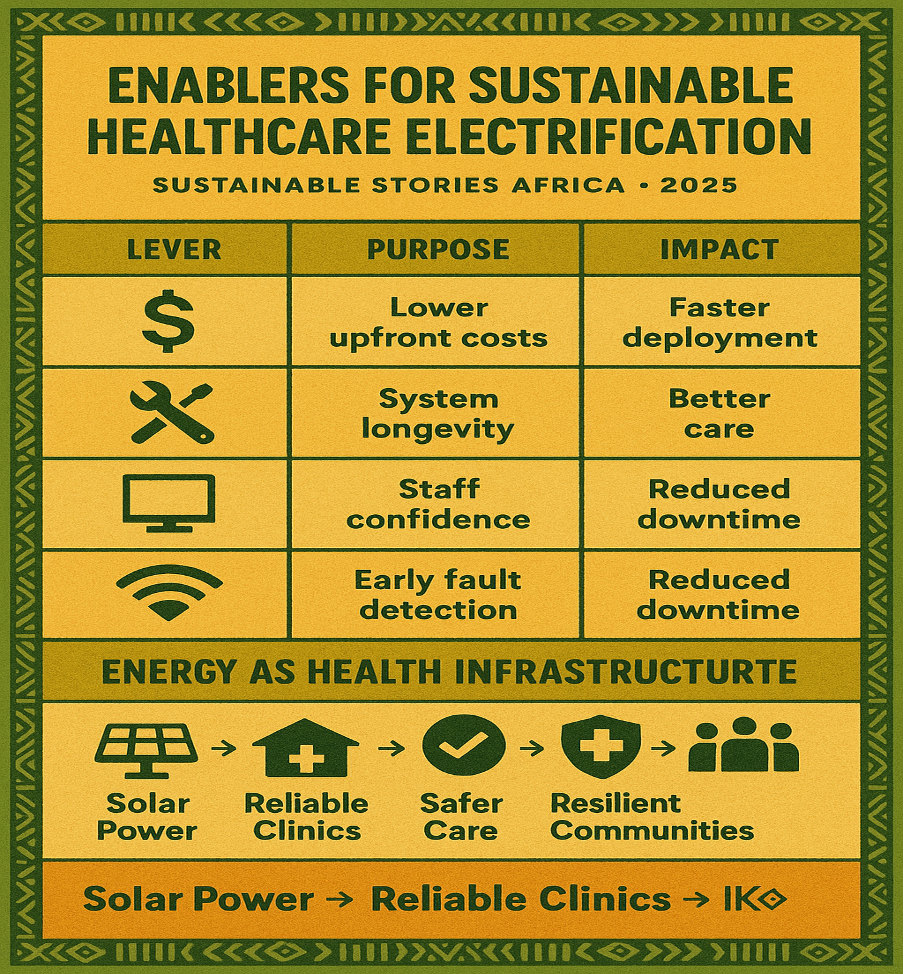
Enablers for Sustainable Healthcare Electrification
| Lever | Purpose | Impact |
|---|---|---|
| Blended finance | Lower upfront costs | Faster deployment |
| O&M funding | System longevity | Reliability |
| Capacity building | Staff confidence | Better care |
| Monitoring systems | Early fault detection | Reduced downtime |
PATH FORWARD – Powering Care, Protecting Lives
Mozambique's healthcare electrification challenge is solvable. With targeted investment, coordinated governance, and decentralised renewables, clinics can move from darkness to reliability, thereby saving lives in the process.
Energy must now be treated as essential health infrastructure. Doing so would strengthen resilience, protect frontline workers, and ensure that climate shocks no longer decide who receives care and who does not.













